Breakthrough in Trauma Care: Rapid Identification and Targeted Treatment Using Molecular Footprints

Rutgers researchers have unveiled a groundbreaking method to rapidly identify and target injury sites in the body, promising faster and more precise trauma treatments. Leveraging the body's molecular response to injury, this innovative approach could significantly improve emergency care outcomes.
Researchers at Rutgers University have developed a revolutionary method for quickly pinpointing injury sites within the body, potentially transforming emergency trauma care. Published in the journal Med, this innovative approach allows for real-time diagnostics and precise treatment delivery in minutes after an injury occurs.
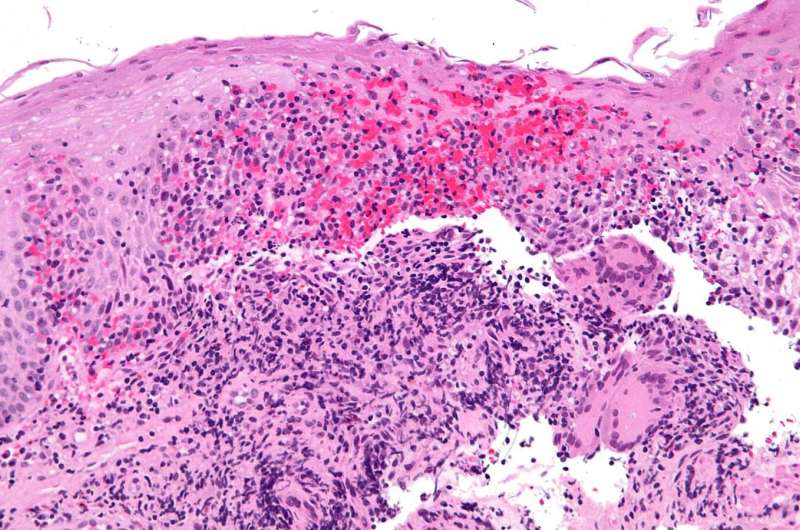
The team, led by Renata Pasqualini and Wadih Arap at the Rutgers Cancer Institute—New Jersey's only NCI-designated Comprehensive Cancer Center—discovered that when cells sustain damage, calcium levels inside them spike, causing specific proteins, termed the "traumome," to change shape. These proteins are exclusive to injured tissues and appear immediately upon injury, paving the way for highly targeted interventions.
This discovery enables the possibility of delivering diagnostics or therapies directly to injury sites without impacting healthy tissues. For example, imaging agents, clotting factors, or antibiotics could be administered precisely where needed, fostering faster healing and reducing side effects. Praising the innovation, Arap remarked, "The instant trauma occurs, specific proteins undergo structural changes, creating a molecular footprint of injury. This opens the door to targeted diagnostics and treatments that minimize collateral damage."
The researchers demonstrated their findings using a pig model with severe injuries, identifying tiny protein pieces called peptides that bind selectively to these altered proteins. One peptide attaches to a protein that changes shape with rising calcium levels following injury. These peptides can be used with imaging techniques like PET or MRI to locate injuries accurately. The same injury signature was observed in rats, indicating broad applicability across mammals, including humans.
The approach is especially promising for treating non-compressible bleeding, a leading cause of pre-hospital death among soldiers and civilians alike. By attaching therapeutic agents to trauma-homing peptides, the method aims to deliver treatments directly to injury sites, improving survival rates. Future steps involve linking drugs and imaging agents to these peptides and testing in animal models before clinical trials.
Arap and Pasqualini envision various applications, from battlefield medicine to civilian trauma care, sports injuries, and surgical recovery. The long-term goal is a simple injection capable of autonomously finding and treating injuries, potentially revolutionizing emergency and military medicine.
Source: https://medicalxpress.com/news/2025-07-identification-method-fast-treatment-trauma.html
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
Discovery of Biological Markers in Mild Crohn's Disease Patients Offers Hope for Personalized Treatments
Researchers at Mount Sinai have identified unique biological signatures in patients with mild Crohn's disease, opening new avenues for personalized treatment strategies and improved disease management.